PINP: A new clinical diagnostic marker of bone metabolism related diseases -Cloud-Clone product reappeared on Nature
Keywords: PINP; Bone metabolism; Tumor; Clinical diagnosis
With the increasing of elderly population in the world, bone metabolism related diseases have become one of the top ten common diseases. Therefore, bone metabolism is a hotspot in medical researches. More and more researchers and clinicians began to look for clinical diagnostic markers of bone metabolism related diseases. Currently, a large number of studies have shown that PINP (Procollagen I N - Terminal Propeptide), a bone formation marker, is closely related to a variety of bone metabolic diseases, tumor bone metastasis and multiple myeloma. And its detection is not affected by food, circadian rhythm, hormones and other interference factors. Therefore, PINP is a new and good clinical diagnostic marker of bone metabolism related diseases.
First of all, let's see some markers of bone metabolism.
Bone metabolism includes bone resorption and new bone formation. Two types of cells are responsible for bone metabolism: osteoclasts (which reabsorb the bone matrix), and osteoblasts (which secrete new bone). Bone decreases due to the absorption of osteoclasts and forms by the synthesis of osteoblasts. There are many metabolites in bone metabolism, which are distributed in bone tissue or body fluids, they affect bone absorption and formation, and maintain the balance of bone metabolism.
There are two kinds of markers for bone metabolism, one is for bone formation, the other is for bone absorption.
1. Bone formation markers mainly include osteocalcin (OC), alkaline phosphatase (ALP), bone alkaline phosphatase (BALP), PINP and Procollagen I C-Terminal Propeptide (PICP).
2. Bone absorption markers mainly include Cross Linked C-Telopeptide of Type I Collagen (CTXI), Cross Linked N-Telopeptide of Type I Collagen (NTXI), Pyridinoline (PYD), Deoxypyridinoline (DPD) and tartrate-resistant acid phosphatase-5b (TRACP5b) [1].
There are so many markers, how to choose?
PINP expression level reflects the formation of new bone. PINP is a byproduct of type I collagen, which is the most prevalent protein in bone. 65% of the bone matrix is inorganic, 35% is organic, and the organic component is mainly collagen type I. In the study of bone formation, measuring byproducts of collagen synthesis is an appealing approach. Following the synthesis of new type I collagen within the osteoblast, PINP is cleaved from type I procollagen by proteases outside the osteoblast. Some PINP deposit directly into the bone matrix, while others enter the blood circulation [2, 3, 4]. When osteoblast synthesis decreased, collagen type I declined, and so did PINP.
The research on PINP is not limited to scientific research, serum PINP monitoring may be particularly clinically useful, reasons are as follows:
1. This marker is relatively insensitive to food and circadian rhythm effects [3, 4, 5].
2. Compared to PICP, PINP is a more specific and sensitive indicator of bone formation, because PINP is not affected by hormones. For the patients with hormone therapy, blood PINP levels were not affected [6].
3. PINP is metabolized by liver, so liver diseases affects its concentration in the blood, but its concentration is not affected by kidney function [7]。
PINP, as a marker of bone metabolism, what is its expression level in different bone metabolism related diseases? What happens to its expression level after treatment?
1. Osteoporosis: After synthetic therapy, expression level of PINP rises.
Osteoporosis is characterized by lower-than-normal bone mass and destruction of bone microstructure, and it increases bone weakness therefore increases the risk of bone fracture. The mechanism of anti-osteoporosis drugs is to promote osteoblast function and inhibit osteoclast function. For osteoporosis patients, total PINP levels were monitored 3 months after treatment with Teriparatide, and 40% increase of total PINP at the basic level indicated that the synthetic therapy was successful. In the treatment of PTH (parathyroid hormone) drugs, PINP increases by about 150% after 3 months [4].
2. Tumor bone metastasis: the expression level of PINP is usually increased.
Tumor bone metastasis diseases are solid tumor metastasize to bone, including prostate cancer bone metastasis, lung cancer bone metastasis, gastric cancer bone metastasis, etc., usually bone resorption and bone formation markers are increased in these diseases. In lung cancer bone metastasis, bone resorption is generally higher than bone formation, while in prostate cancer bone metastasis, the situation is the opposite. Take breast cancer bone metastasis as an example, advanced breast cancer is prone to distant metastasis, bone is the most common metastatic site, accounting for about 70% [8]. When tumor cells migrate to bone, the dynamic balance between bone formation mediated by osteoblasts and bone resorption mediated by osteoclasts will be broken, the expression level of corresponding bone metabolism markers will also be changed. Research has shown that in breast cancer patients with positive axillary lymph nodes, the average level of PINP in tumor bone metastasis is higher than that in those without metastasis [9].
3. Multiple myeloma: the serum PINP level is high, and the expression level of PINP will decrease after treatment.
Multiple myeloma is a cancer of plasma cells, it can cause bone damage, is often accompanied by bone disease [10]. It was found that the serum PINP level in advanced stage patients was higher than that in remission stage patients [2], and the expression level of PINP would decrease after the treatment.
What’s more, diseases involving high bone turnover would be expected to be associated with high concentrations of PINP. Examples are metabolic bone diseases including osteomalacia and Paget’s disease, endocrine disorders including thyrotoxicosis and primary hyperparathyroidism, etc [2, 4].
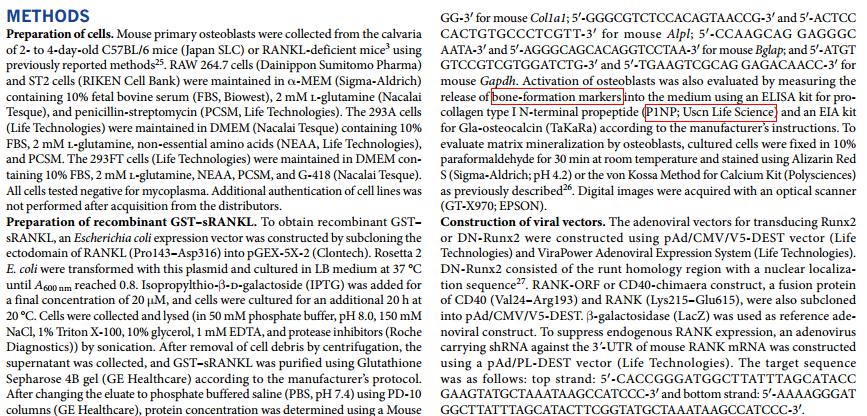
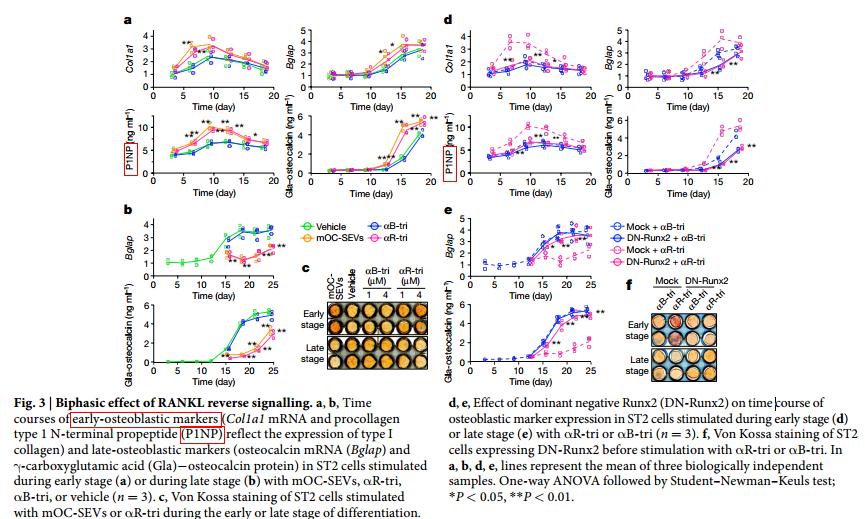
With the increasing popularity of bone metabolism research, the detection requirement of PINP expression level also increases. For our PINP ELISA products, there are 39 citations. Most of the researchers tested PINP because it is bone metabolic marker, including a paper which is published in Nature magazine in September, 2018, the title is "Coupling of bone resorption and formation by RANKL reverse signalling", the researchers used a mouse ELISA kit from Cloud-Clone to detect bone formation marker - PINP[11]. Part of the methods and results are shown below. This also reflects the researchers' recognition of PINP as a marker of bone metabolism.
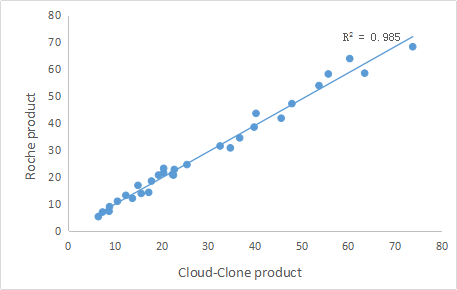
More than that, based on the characteristics of PINP itself and its advantages in clinical research, PINP has been widely used as a biochemical indicator of bone metabolism in clinic. For example, it has been applied to the prediction of fracture risk degree, monitoring of bone loss rate, differential diagnosis of metabolic bone disease and monitoring of drug treatment response. Therefore, PINP can be used as a new and feasible clinical diagnostic marker for bone metabolism related diseases. More and more clinicians also began to look for high-quality IVD materials or IVD reagents of PINP to meet the needs of clinical diagnosis. After continuous efforts, Cloud-Clone developed IVD raw materials of high quality, these products have been verified by a third-party, and their experimental performance are consistent with Roche’ product’s . Part of experimental results are shown below:
It is hoped that our products can be helpful for bone metabolism research and clinical diagnosis of related diseases.
For more information, please visit: http://www.cloud-clone.com/
1. Kanabrocki EL, Hermida RC, Wright M, et al. Circadian variation of serum leptin in healthy and diabetic men. Chronobiol Int, 2001; 18(2):273-283.
2. Vasikaran S, Eastell R, Bruyère O, et al. Markers of bone turnover for the prediction of fracture risk and monitoring of osteoporosis treatment: a need for international reference standards. Osteoporos Int, 2011; 22(2):391-420.
3. Terreni A, Pezzati P. Biochemical markers in the follow-up of the osteoporotic patients. Clin Cases Min Bone Metab, 2012; 9(2):80-84.
4. Krege JH, Lane NE, Harris JM, et al. PINP as a biological response marker during teriparatide treatment for osteoporosis. Osteoporos Int, 2014; 25(9):2159-71.
5. Naylor K, Eastell R. Bone turnover markers: use in osteoporosis. Nat Rev Rheumatol, 2012; 8(7):379-389.
6. Hernandez MV, Guanabens N, Alvarez L, et al. Immunocytochemical evidence on the effects of glucocorticoids on type I collagen synthesis in human osteoblastic cells. Calcif Tissue Int, 2004; 74: 284-293.
7. Ureña P1, De Vernejoul MC. Circulating biochemical markers of bone remodeling in uremic patients. Kidney Int, 1999; 55(6):2141-56.
8. Mundy GR. Metastasis to bone: cause, consequences and therapeutic opportunities. Nature Reviews Cancer, 2002; 2(8):584-593.
9. Jukkola A, Bloigu R, Holli K, et al. Postoperative PINP in serum reflects metastatic potential and poor survival in node-positive breast cancer. Anticancer Res, 2001; 21(4B): 2873-2876.
10. Kyle RA, Gertz MA, Witzig TE, et al. Review of 1027 Patients With Newly Diagnosed Multiple Myeloma. Mayo Clin Proc, 2003; 78(1):21-33.
11. Ikebuchi Y, Aoki S, Honma M, et al. Coupling of bone resorption and formation by RANKL reverse signalling. Nature, 2018; 561(7722):195-200.
